Two directions to go, many turns to take: Ludmila´s second research stay at Italy
Advancing in her professional skills and learning new research methods are the two outcomes that Ludmila Zarska points out as the most important benefits from her three-month-long research stay at ISTEC, the partner´s laboratory in Italy. Ludmila is one of the two PhD students involved in Nano4Tarmed research. The focus on young researchers driven by the need to develop future leaders with a capacity for interdisciplinary and international working is one of the main objectives of the project. Jan Belza, the second N4T postgraduade student, is getting ready for another of his research stays in Ireland in October.
The ISTEC laboratories weren´ t new territory for Ludmila. She joined their team for a month last Fall to test if the bioconjugated graphene flake nanocarriers designed to detect and directly target the cancer cells exhibit the desired outcomes. What are the new findings?
Nanocarriers upgraded
„Last time, I brought with me for testing to ISTEC the nanocarriers consisting of graphene-oxide flakes wrapped in PEG, polyethylene glycol, with bioconjugated cisplatin. After my return, I worked on configuration of the platform. We added doxorubicin, a common cancer beater, into the composition hoping that synergies between the two functional drug components could occur. Additionally, we added hyaluronic acid into the mix to help with binding a higher drug concentration to the platform. It is also a well-known fact that this acid binds to CD44 protein present in the cancer cell membranes. We wanted to take advantage of this Achilles heel of the damaged cells,“ says Ludmila about her research work and prepares for the second stay.
Challenge of unknown
At ISTEC laboratories, the team tested this loaded „package“ on 2D cell cultures of the two glioblastom tumor lines (the type of brain tumor). One with higher and one with lower level of the CD44 protein. „What we found out was that doxorubicin was the strongest player of this mix. The rest of the composition didn´t play a significant role,“ explains Ludmila.
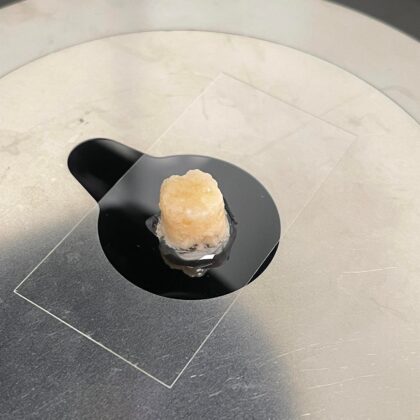
Another step was to observe the efficiency on 3D cell models using a scaffold method. „Scaffold is a material with porous sponge-like structure, primarily used in tissue engineering. It can be composed of collagen, for example, with some additives helping cells to grow,“ she describes.
First, the cancer cells were applied on the scaffold. A week later, the drug was added. „We let it work for three days and then evaluated how many of the cells survived. Unfortunately, we didn’t get any positive results out of this experiment,“ says Ludmila. „The number of cells that died with or without an application of the drug was the same. There are still many factors to optimize and to find out. For example, how does the scaffold material influence the whole process? Does it interact with the cells? With the hyaluronic acid? And how? Doesn´t the acid create an enclosure disabling the active agent to be released? We cannot simply figure this out with some device, under the microscope. It is a trial-and-error process with many variables.“
Blind route and its benefits
„We learnt what route not to take. That was a valuable finding of this experiment. During the process, I learnt working with the scaffolds, got familiar with cell planting, and advanced my microscoping skills. Colouring the samples for example. One has to understand how to properly apply the colorant detecting the cancer cells otherwise everything will get coloured. We also examined scaffold cuts and evaluated how the cells grew in there. This was new for me as well.
Now, to progress further, we either figure out how to better target the platforms to the damaged cells or we change the combination of the drugs. There are not many other ways to go. But variables are many,“ concludes Ludmila.